Hypothermia
This will focus on accidental hypothermia; there
are numerous secondary causes that will not be the focus of this review.
Although typically associated with regions of the
world with severe winters, hypothermia is also seen in areas with warmer
climates, as well as during summer months and in hospitalized patients. Even with modern supportive care, mortality
for patients with moderate to severe accidental hypothermia approaches 40%.
Body Temperature reflects the balance between heat
production (cellular metabolism) and heat loss (evaporation, radiation,
conduction & convection). The normal
human core temperature is 98.6±0.9oF (37±0.5oC). The human body has limited physiological
capacity to respond to cold environmental conditions (basically, peripheral
vasoconstriction), thus our behavioral adaptations of clothing and
shelter. In response to a cold stress,
the hypothalamus attempts to stimulate heat production through shivering and
increased thyroid, catecholamine and adrenal activity. There is also sympathetic mediated
vasoconstriction of peripheral tissues.
Hypothermia is
defined as a core temperature below 95oF (35oC).
- Mild: 93.2 – 95oF (34-35oC)
- Moderate: 86 – 93.2oF (30-34oC)
- Severe: less than 86oF (less than 30oC)
Mild hypothermia is characterized by
tachypnea, tachycardia, initial hyperventilation, ataxia, dysarthria, impaired judgment,
shivering and “cold diuresis.” “Cold Diuresis” is renal-fluid wasting due to hypothermia-induced vasoconstriction
and diminished release of anti-diuretic hormone.
Moderate hypothermia is
characterized by a proportionate reduction in pulse rate and cardiac output,
hypoventilation, central nervous system depression, hyporeflexia, decrease
renal blood flow, and the loss of shivering.
Patients may begin to display paradoxical undressing. Atrial fibrillation, junctional bradycardia
and other cardiac arrhythmias may also occur.
Patients with severe hypothermia
develop pulmonary edema, oliguria, areflexia, hypotension, bradycardia, coma, ventricular
arrhythmias and asystole.
Risk Factors for hypothermia include: Age (infants
and the elderly), Environmental (exposure, drowning, and an alpine
environment), Poverty, Homeless, Drugs / Toxicology and Psychiatric disorders.
To measure the temperature in a hypothermic
patient requires a low-reading thermometer.
Most standard thermometers only read down to 93oF (34oC). If the patient is conscious, a rectal probe
thermometer is practical (although, to be truly accurate, needs to be inserted
15cm). If the patient is intubated, an esophageal
probe is preferred and is most accurate (inserted into the lower 1/3 of the esophagus).
What studies to obtain?
- Finger stick glucose! Do not miss the patient who is hypothermic secondary
to hypoglycemia. Remember, if the
patient does not have glucose, the body cannot generate heat to help rewarm
itself. Also, insulin release is
decreased in hypothermia, so hyperglycemia is common.
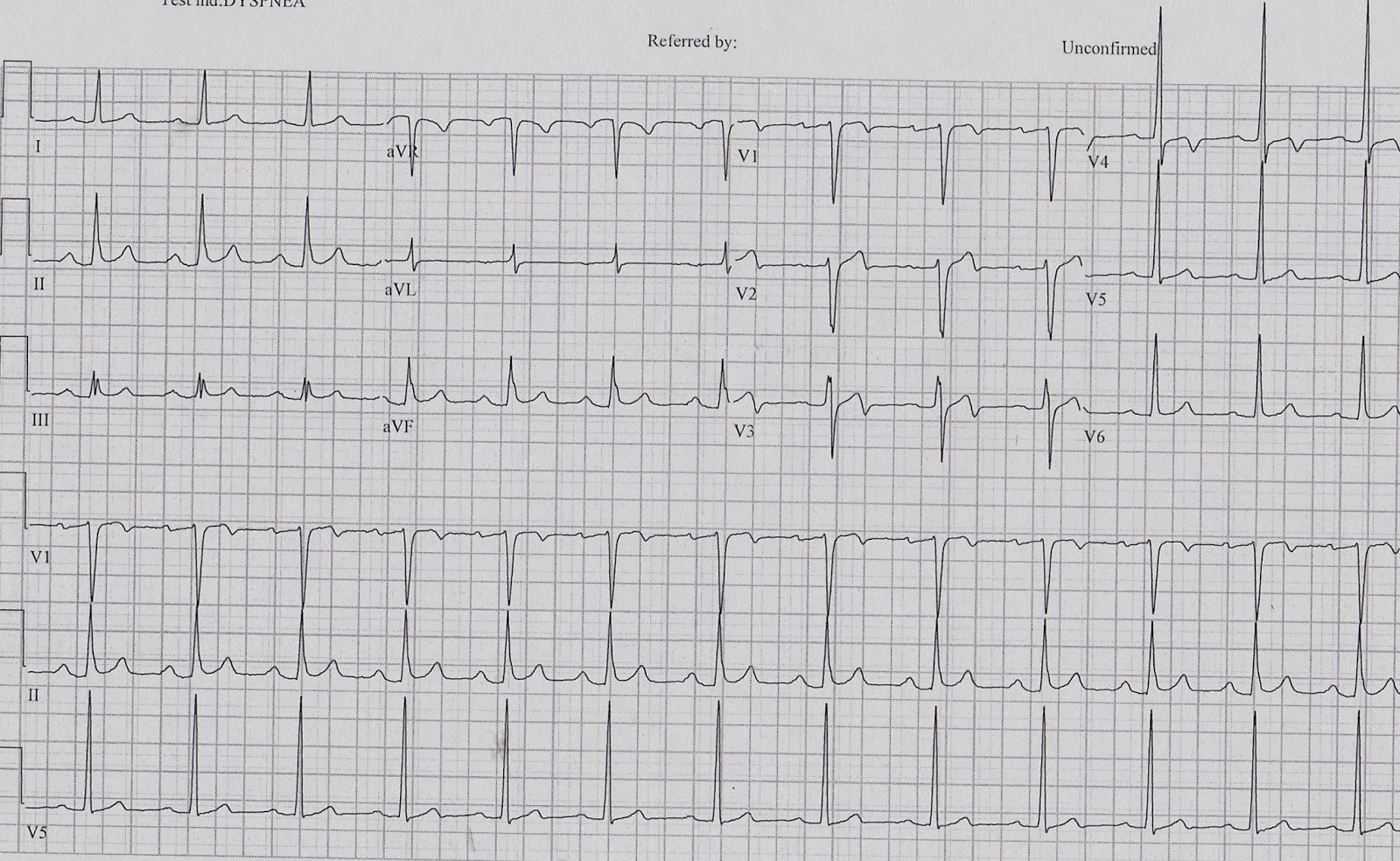
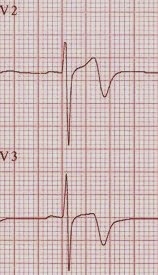
- ECG
- Hypothermia
causes characteristic ECG changes because of slowed impulse conduction through
potassium channels. This results in
prolongation of all the ECG intervals.
There also maybe elevation of the J point, producing the characteristic
Osborn J Wave (from the distortion of the earliest phase of membrane
repolarization).

- BMET
- Resuscitation
is futile if K >10
- Check
frequently during the resuscitation
- CBC
- There
is 2% drop in Hct for each 1oC drop in temp
- Thrombocytopenia
is common
- Lactate – elevated from shivering and poor
tissue perfusion
- PT/PTT – often coagulopathy is clinically evident
but laboratory studies appear normal as the test is run at 98.6F (37C)
- Fibrinogen
- Creatine phosphokinase
- Arterial blood gas – acidosis often present due
to severe respiratory depression and CO2 retention as well as lactic
acid production
- CXR – pneumonia (aspiration) is a common
complication
- Toxicology screen
- ETOH
Management
- ABCs
- There is an alteration in ACLS algorithm for
patients with severe hypothermia (less than 86oF (less than 30oC)). In patients with severe hypothermia, begin
CPR and attempt defibrillation once. Withhold
typical ACLS medications and any further defibrillation attempts until the patient’s
core temp is >86oF (>30oC). These patients will require active internal
rewarming (information below).
- Peripheral pulses may/will be difficult to
assess, check a central pulse for up to a minute and consider using doppler.
- Establish two large bore (14 or 16 gauge)
peripheral intravenous lines and start an infusion of warmed (100.4 – 107.6oF
(38 – 42oC)) isotonic crystalloid.
This will only really prevent further heat loss! If central venous access is needed, use the
femoral approach, if possible (to avoid the guide wire irritating the right
atria and causing an arrhythmia, which can occur with the internal jugular or subclavian
approach).
- Treatment of cardiac arrhythmia. Handle these patients with care! Movement has been reported to trigger
arrhythmias, including lethal ventricular fibrillation. Remember, bradycardia is expected and pacing
is not required unless the bradycardia persists despite rewarming to 90-95oF
(32-35oC).
- Typical
progression is sinus bradycardia to atrial fibrillation to ventricular
fibrillation to asystole.
- Rewarming Therapies
o Passive
External Rewarming (PER). This is the
treatment of choice for patients with mild hypothermia. Removal all wet and cold clothing and then
cover the patient in blankets or other types of insulation (aluminum foil). Set room temp to 82oF. PER
requires the patient to have a physiologic reserve sufficient to generate heat
by shivering and an increased metabolic rate.
If the patient’s temperature does not rise by 0.5-2oC/hr.,
reconsider the diagnosis (are they septic, hypoglycemic, hypovolemic, endocrine
source, etc.) and consider starting AER.
o Active
External Rewarming (AER). AER is
indicated for moderate to severe hypothermia and for a patient with mild
hypothermia who is unstable, lacks physiologic reserve or fails PER. AER is a combination of warmed blankets, heating
pads (watch for body surface burns from decreased sensation and reduced blood flow),
radiant heat, warm baths, or forced warm air, which are applied to the patients
skin.
§
Core Temperature After Drop is a risk during
AER. This occurs when the truck and
extremities are warmed simultaneously.
Cold, academic blood that has pooled in the extremities returns to the
core and can cause a drop in temperature and pH. This can trigger cardiac dysrhythmias.
§
Rewarming shock can occur when peripheral
vasodilation and venous pooling results in relative hypovolemia and
hypotension.
o Active
Internal Rewarming is indicated for severe hypothermia and those who fail to
respond to AER.
§
Airway rewarming is utilized by use humidified
air at 40-45oC.
§
Pleural irrigation can be accomplished by
placing two thoracotomy tubes (36 to 40 French), one placed anterior and one
posterior, and instilling warmed IVF into the anterior chest tube and allowed
to drain out the posterior chest tube.
If the patient is pulseless, use the left thoracic (bath the heart in
the warm fluid), if the patient has a pulse, use the right thoracic to avoid
triggering an arrhythmia by irritating the heart with tube insertion.
§
Bladder irrigation is another option
o Extreme
options (not readily available in many EDs): ECMO, hemodialysis, cardiopulmonary bypass
o Glucose,
if the patient is hypoglycemic
o Naloxone
o Thiamine,
as patients are often alcoholics (also, Wernicke’s)
o Hydrocortisone,
if the patient has a history of adrenal insufficiency
o Antibiotics,
for suspected sepsis
Remember, the patient is not dead until they are
“warm and dead.” But, how warm is warm? Target a temperature of 89.6oF (32oC)
in adults and a temperature of 95oF (35oC) in
children.
If the body is frozen and chest compressions are
impossible; or if the nose and mouth are blocked by ice; or if the patient’s
potassium is >10, then resuscitation can be withheld.
References:
Tintinalli Sixth Edition
Accidental hypothermia in Adults. Up-To-Date
Circulation. 2005;112:IV-136-IV-138.
Brown, et al. Accidental Hypothermia. N Engl J Med
2012;367:1930-8.