Ok, so not every post on EverydayEmergencyMedicine will
focus on the basics, some will focus on the rare/odd/funny cases that we see
everyday as well.
Case Presentation:
Sorry, the blog post title gives the case away….
Male in his early 50s presents for a sexual transmitted
infection (STI) check, along with his new (and younger) significant other; he
is currently asymptomatic. During the history,
patient admits to some shortness of breath and chest discomfort during a recent
argument with his significant other, as well as, some shortness of breath with
exertion (both walking and intercourse) in the past few days. Patient, again, has no current complaints.
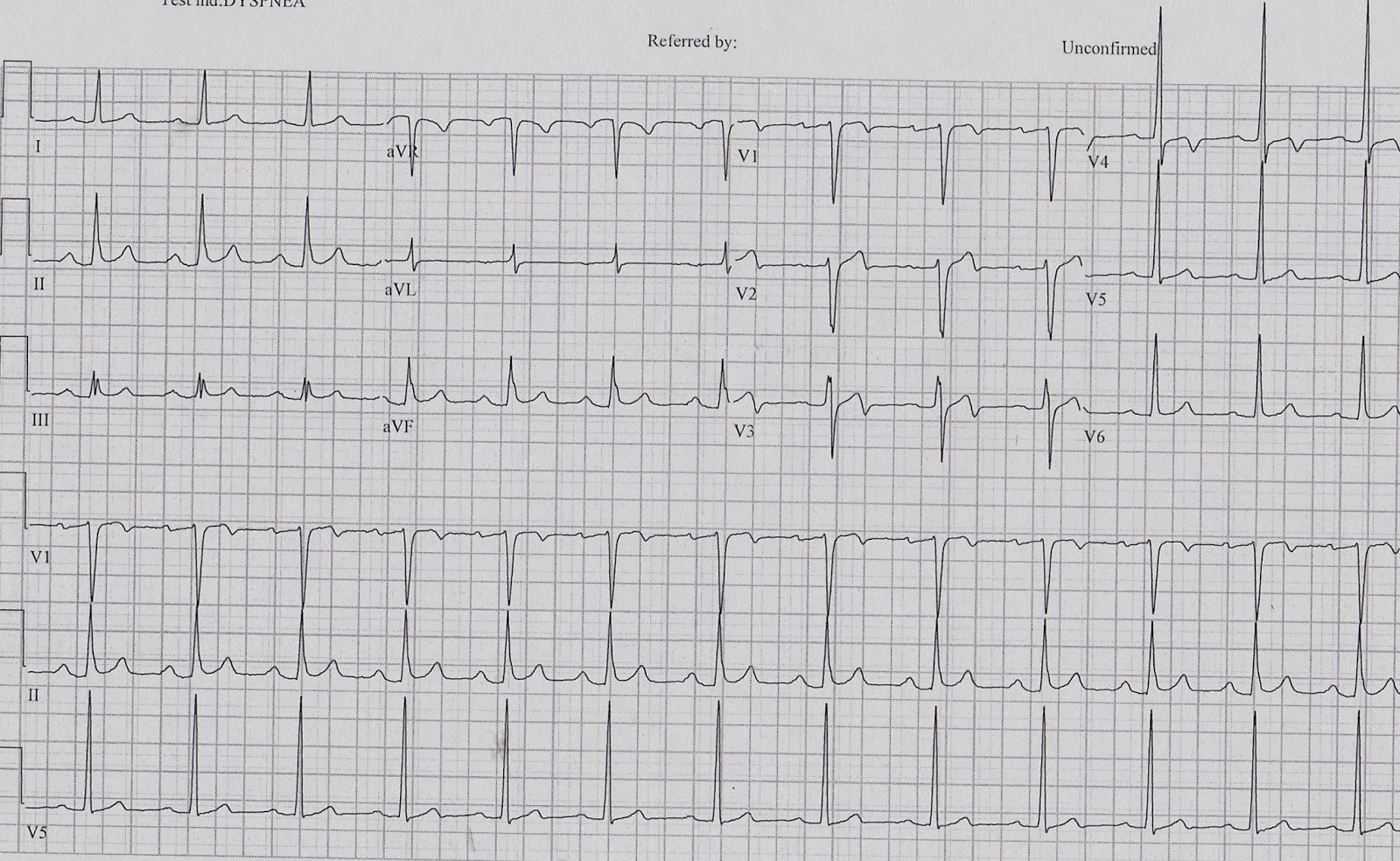
The history prompted the patient to have an ECG preformed. Which showed….
Because of these findings, cardiology was contacted and the
patient was admitted.
What does this ECG show?
… Wellens Syndrome
Wellens Syndrome represents a characteristic T-wave change
on electrocardiogram (ECG) that is present during pain-free periods in a
patient with intermittent chest pain and symptoms consistent with unstable
angina/ischemic chest pain.
The findings of Wellens Syndrome suggest a high-degree
stenosis of the proximal left anterior descending (LAD) coronary artery (i.e., the
“Widow Maker”), that if not treated with intervention will lead to a massive
anterior myocardial infarction and/or death within two weeks (mean time, 8.5
days) in 75% of patients (i.e., a “Widow Maker”). Medical Management is ineffective.
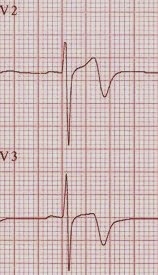
Wellens syndrome is characterized by T-wave changes in the
precordial leads, mainly V2 & V3 ± V4, during pain free periods, in a patient with a history of chest pain that
is consistent with unstable angina/ischemic chest pain. Type A (or Type I) (75-76% of cases) shows
deeply inverted T-waves, while Type B (or Type II) (24-25% of cases) shows biphasic
T-wave. Type A is rarely missed, but Type
B is often interpreted as “non-specific T wave changes” by the computer and
clinicians.
Type A (or Type I)
Type B (or Type II)
The diagnosis should be made by the history obtained from
the patient and ECG only, as cardiac enzymes will be normal or only mildly
elevated. This also helps enforce the
importance of serial ECGs and pain-free ECGs in patients with a history of
chest pain that is concerning for unstable angina/ischemic chest pain.
These patients do not necessarily need immediate catheterization,
but they need urgent catheterization. These
patients should not undergo a stress
test, as it places them at risk for an acute anterior wall myocardial
infarction. Cardiac catheterization has
demonstrated patients with Wellens syndrome to have a 50% or greater stenosis
of the proximal LAD.
Case resolution:
This patient’s ECG showed Wellens Type B (or Type II) … biphasic
T waves in leads V2 & V3 (and arguably in leads in V1 & V4 as well),
the computer read it as “T wave abnormality, consider anterior ischemia.” The patient was asymptomatic in the emergency
department and had negative cardiac markers and was admitted to cardiology (the
patient was reluctant to be admitted). Cardiology
did order a treadmill stress test for the morning, which the patient failed and
thus went to cardiac catheritzation and a 95% proximal LAD lesion was found and
two stents were placed.
Had this been missed, the patient likely would have
passed in bliss during intercourse with his younger significant other (personal
commentary).
References:
Rosen’s 7th Edition
De Zwaan C, Bar FW, Wellens HJ. Charcteristic
electrocardiographic pattern indicating a critical stenosis high in the left
anterior descenting artery in patients admitted because of impedning myocardial
infarction. Am Heart J. 1982;103:730-6.
J Emerg Trauma Shock. 2009 Sept Dec; 2(3): 206-208.

No comments:
Post a Comment